I am often asked what my most common exercises are for my patients depending on their ailments. I decided to put this list together for you. Make sure you check out my most common stretches as well.
Deep neck flexors
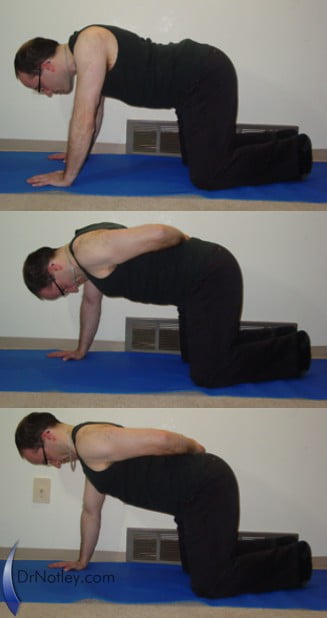
The deep neck flexors are at the front of the spine, immediately in front of the vertebrae. These muscles are often weak and inhibited after a motor vehicle accident. They are also inhibited and deconditioned if you sit or stand all day with your head forward in front of your shoulders. These muscles are associated with a flattening of the cervical spine (loss of it’s natural backwards curve) or a reversal of the cervical spine (forwards curve; kyphotic). The neck retraction exercise to help stretch out the suboccipital muscles helps to activate the deep neck flexors as well. Another more challenging exercise for the deep neck flexors is the quadruped neck retraction exercise (note: arm is behind back only to show movement of neck). You can build on this exercise by adding resistance by using tubing draped over the head and held by the hands). You can also work on the neck retraction followed by turning the head as in this video.
Rhomboids and Trapezius muscles
The rhomboids are often over looked. It is rather easy to over look then because they are found on our back side between our shoulder blades. These muscles are often inhibited by inactivity and are cause of rounding of the shoulders. Poor activity of these muscles means poor mechanics at the shoulder which can lead to shoulder injuries such as impingement syndrome or shoulder bursitis. To train these muscles I perform T’s and Y’s. My favorite piece of exercise equipment to perform these two exercises on the TRX suspension trainer, but you can also use elastic exercise tubing.
Serratus Anterior
Serratus anterior is found on the side of our ribcage and travels up into our armpit and attaches to our shoulder blade. One of the jobs of this muscle is to hold the shoulder blade against our ribcage. Weakness of these muscle leads to our shoulder blades popping up off of our rib cage as we do a pushup. Another job this muscle has is to aid in abducting out shoulder blades as we raise our arms over head. Any weakness or dysfunction in this muscle can cause a movement dysfunction at the shoulder which can lead to shoulder injuries. The scapular pushup is an excellent way to start training this muscle. If you can’t perform it on the floor then try performing it against a wall or with your elbows on a bed/bench. Check out this video as well
Four for the Core
As mentioned in my previous blog post, the plank, side plank, bridge and the McGill crunch are my four preferred exercises to give to my chiropractic patients. Check out my Four for the Core here
Tibialis anterior (shin muscles)
The muscles at the front of the shins are responsible for lifting the foot up. They are also responsible for aiding in maintaining the arch in the foot while walking or running. strengthening these muscles so they can handle the repetitive strain of long walking or running is important for preventing walking/running injuries such as shin splints. Perform this exercise by standing with your back resting on the wall and feet out from the wall. The further away from the wall you are the harder the exercise will be, especially if you have a shoe with a heel. With the body straight, lift toes up off the ground.
Make sure to take a look at my blog post on starting exercise and preventing injury.
Originally posted on May 17, 2022 @ 4:40 pm
